The National Clinical Advisory Team Report on the future of Calderdale and Huddersfield A&E, commissioned by Calderdale and Huddersfield NHS Foundation Trust, is now in the public domain after months of secrecy.
This is what its guff about “delivering more care outside the hospital“, “community-focussed care“, “putting the patient first” and “transformation” really means: yesterday £1,222,000,000.00 of our NHS was offered up to Private Health by
NHS Greater East Midlands Commissioning Support Unit,
“Commissioners are seeking genuine, transformational and sustainable service change that recognises the primacy of the patient in the service model…” (links to the contract advertisements are at the end of this article)
West and South Yorkshire and Bassetlaw Commissioning Support Unit will be following hard on their heels if we let the CHFT Strategic Review (which is based on the NCAT Report) go through.
The NCAT Report bangs on about staff shortages as the “key driver” for closing one A&E department and siting all A&E in one hospital, but misses the opportunity to say that these staff shortages are unacceptable and need sorting.
The NCAT Report appears to be driven by an unacknowledged cuts and privatisation agenda, while foregrounding claims that its recommendations are based on clinical judgements.
It says that the fit with future funding has been a consideration. But it doesn’t discuss the ongoing NHS funding cuts that drove Calderdale CCG to ask CHFT to commission the NCAT Report, and it warns that the options it considers will cost a lot, in terms of extra staff and/or capital investment.
Imo, the NCAT Report is more notable for what it doesn’t say than what it does say. It doesn’t say that its recommendations for reducing hospital beds and increasing care in the community align closely with NHS England Chief Sir David Nicholson’s remedy for the £30bn NHS “funding gap” that will open up by 2020/21. According to Sir David N:
“This gap cannot be solved from the public purse but by freeing up NHS services and staff from old style practices and buildings.”
It acknowledges that its recommendations for reduced cover at one hospital site will
“present significant challenges over opening hours, workforce, clinical dependencies, handovers and public perceptions.”
Weirdly, in a set of proposals that aim to put the patient first, the NCAT Panel did not hear from any patient representatives.
The NCAT Report advocates:
- All A&E in one acute care hospital – meaning that consultant-delivered obstetric care, paediatric medical and surgical and neonatal services would all go there too. This decision is driven by national and regional shortages in A&E consultants and mid-grade paediatricians; CHFT’s current inability to staff A&E at levels that comply with College of Emergency Medicine standards; and high cost to CHFT of employing locums to make up staffing shortfalls.
- Unplanned care in the other hospital
- Minor Injuries Units in both hospitals
- Something quite unspecified in Tod Health Centre
- Reduce hospital beds, keep patients out of hospital and treat them outside hospital instead – particularly children, the elderly and people with chronic health problems
- Expand Locala-type community health care
- Increase use of digital technology and shared patient data, in patient care and commissioning
The NCAT Report recommendations split into two groups. One is about the future of A&E, the other is about how to reduce A&E admissions.
Future of A&E
NCAT recommends putting all A&E on one acute care site, and says the choice of whether to site this at Calderdale Royal Hospital or Huddersfield Royal Infirmary is “a local management decision”.
(So, in the eyes of NCAT, CHFT managers have the say, not the Secretary of State for Health who, as a result of the 2012 Health & Social Care Act, no longer has a duty to provide universal, equitable health care that is free at the point of need.)
The NCAT Report says that staff shortages in A&E are the main reasons for recommending putting all A&E on one acute care site.
A member of the NCAT Panel commented,
“The key driver for change is that it is not possible to maintain A&E sites at both CRH and HRI on a 24/7 7 day a week basis. Expected standards of consultant delivered care cannot be met and the 2 A&E services are already under pressure to function due to rota vacancies particularly at middle grade. There is a significant reliance on locums.”
The NCAT Panel member said that putting all Emergency Department (ED) services on one site, with a Minor Injuries Unit on the other site, would solve the problem that CHFT does not meet College of Emergency Medicine staffing levels , and this is
“the principal advantage of this reconfiguration model.”
Shortage of Paediatric doctors leads to the judgement in the Women and children presentation that:
“Separate site or status quo model… will not be safe and/or sustainable. Medical workforce is the big issue that Paediatrics will face…obstetrics and neonatal care should also be on a one site acute hospital service.”
The Women and children presentation states that the problem will get worse because there will be,
“Drastic reduction in Specialist Training in Paediatrics starting August 2014”
Paediatric Senior House Officers in the region will drop to 41 compared with 136 currently. Middle grade Paediatric doctors in the region will drop from around 204 now to 55. At the moment CHFT needs 11 middle grade Paediatric doctors but “at best only 2-3 in post at CHFT.”
The Medicine presentation is almost all about cost savings and staffing rationalisation that would result from a single site A&E with Medical and Acute Oncology Services on the same site.
The Medicine presentation also refers to
- Potential safety and quality improvement opportunities.
- Reduced risk of ambulance transfer breaches (impact on 4 hour performance).
And it notes that
“both clinical and managerial leaders of this clinical division would recommend a single site for acute care.
Hospital Standardised Mortality Ratio- CRH had 24 more pneumonia deaths than the model predicts; this is more than the calculated “excess” deaths for the Trust as a whole for this period, in the 56 diagnostic groups of HSMR. The HSMR difference between CRH and HRI is not just confined to pneumonia. On review there appears to be a failure of systems not of individual care.”
What the NCAT Report says about reducing Calderdale & Huddersfield A&E admissions
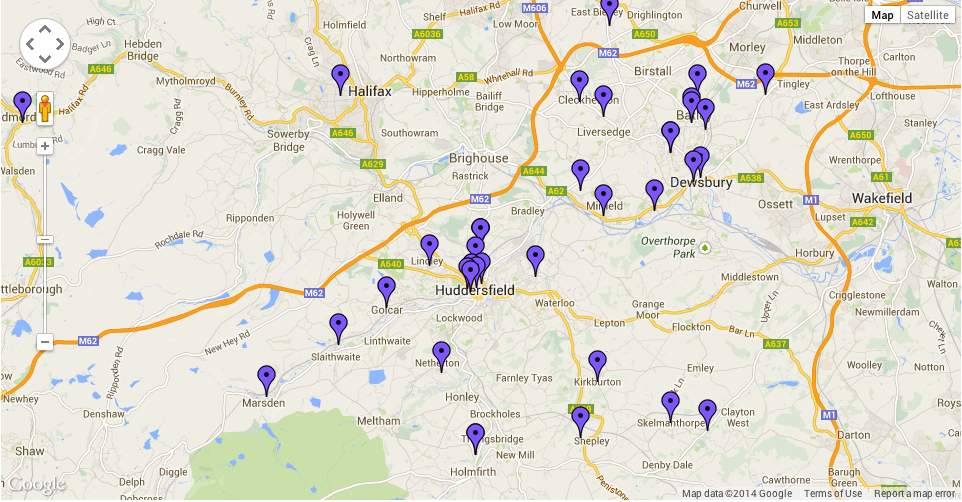
The NCAT Report recommends big changes to the whole of Calderdale & Huddersfield primary care NHS and social care services, as a way of reducing patients’ need to go to A&E.
The NCAT Report doesn’t say that the need to reduce the number of patients going to A&E is driven by NHS funding conditions: Calderdale CCG is only allowed to pay CHFT 30% of the tariff for any A&E admissions over the 2008/9 baseline. It has to spend the 70% left over on “relevant demand management schemes” and it will have to publish its plans for demand management.
Maybe NCAT assumed that everyone already knows this.
The NCAT Report recommends these measures to reduce A&E admissions:
- enhancing primary and community based services to deliver more care out of hospital
- implementing “community focused options, GP access to the community paediatric service, the continuing development of community based services for those patients who have a long term condition. The systematic adoption of case management, risk stratification methodology and multidisciplinary teams working with general practice and the implementation of the proposed virtual wards.” (This set of recommendations needs unpicking, and I’ve tried to start doing this in the next section)
- Shared clinical records and clinical pathways across two hospital sites and with community based services
“Community-focussed options”
There is a massive amount to unpick in this set of recommendations, so I’ll only make a bit of a start here.
The recommendations I want to focus on are the ones that seem to advocate an extension of Locala-type community health care.
Locala is a private social enterprise company that spun off from Kirklees Primary Care Trust (PCT) (an organisation that no longer exists due to the Health and Social Care Act 2012, which abolished PCTs).
Like Foundation Trusts and Commissioning Support Units, it is not accountable under the terms of the Freedom of Information Act. As a company it can claim commercial confidentiality.
It runs a load of community health services in Kirklees, such as district nursing, health visitors, stop smoking services and has a big presence at Holme Valley Memorial Hospital, Holmfirth. It also has the interim contract for Park Ward and Todmorden walk in centres.
The NCAT Report says that Locala has a good relationship with GPs and uses risk stratification methodology.
Risk stratification methodology is a technique promoted by the Nuffield Trust, a pro-NHS privatisation think tank. It uses computer models for analysing hospital and GP medical records to predict demand for unplanned hospital admissions and to help determine health payments – either for fixing ‘capitated’ budgets or for deciding reimbursement rates for individual patients. (This relates to proposals to pay for healthcare through personal budgets, which is a whole other can of worms.)
One computer model, PARR, has been used widely across England to identify patients that should be offered hospital avoidance support, such as care from a Community Matron
Again using Nuffield Trust information, Virtual Wards are a system for offering “hospital avoidance support”, using the same staffing, systems and daily routines as hospital wards, except that the people being cared for stay in their own homes throughout.
A Nuffield Trust evaluation of Virtual Wards in Devon, Croydon and Wandsworth, compared with matched controls,
“found no evidence of a reduction in emergency hospital admissions for patients who received this type of care in the six months after starting the intervention. Nor did we find evidence of a reduction in ambulatory care sensitive hospital admissions or mortality in this period”.
So maybe it’s not such a great way to reduce A&E admissions.
Who did and didn’t have a say in the NCAT Report on Calderdale and Huddersfield A&E
The 3-person NCAT Panel spent one day hearing and discussing presentations from CHFT, Yorkshire Ambulance Services, Greater Huddersfield and Calderdale Clinical Commissioning Groups and a couple of NHS groups from neighbouring areas. It also read a number of documents. They then wrote their Report.
Although the NCAT Report recommends huge changes to GP and community care health and social care services, only one Calderdale GP took part in the presentation by GPs and CCGs on urgent care in primary care. This was Dr Majid Azeb of Southowram Surgery, Care Quality Commission member (and of M & N Medicals Ltd ). Dr Azeb is the urgent care lead on Calderdale CCG.
No patient representatives had a voice in the discussions and presentations to the NCAT Panel
No patient representatives or political representatives of local people had a voice in the discussions and presentations to the NCAT Panel. A Calderdale Councillor made an unsuccessful FOI request to see the Report last summer summer. Calderdale 38 Degrees asked Calderdale CCG what was going on. Linda Riordan MP asked the Under Secretary of State for Health what was going on.
The Under Secretary of State made out that the Department of Health had no say in the discussions, on the grounds that this was a matter for local clinical judgements.
As if.
What the NCAT Report doesn’t say – the hidden cuts and privatisation agenda
The NCAT Report doesn’t say anything about cuts to NHS and social care funding which lie behind Calderdale CCG’s decision to ask CHFT to review the future of A&E in Calderdale and Huddersfield, as stated by CCCG’s Chief Officer Matt Walsh at a Calderdale CCG meeting.
NHS England requires Calderdale Clinical Commissioning Group to cut its spending on
Calderdale NHS by 4% of its budget each year, through so-called efficiency savings. On
top of that cut, West and South Yorkshire and Bassetlaw Commissioning Support Unit have planned an extra £160m cut.
The NCAT Report does not say anything about the costs of carrying out the Health & Social Care Act 2012, which take a sizable chunk out of NHS spending on health care services.
Dr Louise Irvine, chair of Save Lewisham Hospital Campaign, has estimated that the
administrative costs of managing the full-blown competitive provider market unleashed by
the Health and Social Care Act could rise to over 20% of the NHS budget for England.
That would mean that over £15 billion a year would be spent on managing the market –
money that will have to be found in addition to the £20 billion over 4 years so-called
efficiency savings.
The NCAT Report doesn’t say anything about additional NHS funding cuts imposed by NHS England in July 2013
(To be fair, this was announced after the NCAT Panel hearing, but they could have drawn
attention to it if they’d been so minded, as an addendum or something.)
In July 2013, NHS England told Clinical Commissioning Groups (CCGs) to save £30bn over the next 3-5 years, in addition to the £5bn/year efficiency savings they already have to
make over 4 years. As already noted, these efficiency savings represent 4% of the CCGs’
annual budget.
The NHS England document, laughably called “The NHS belongs to the people: a call to
action”, tells CCGs to come up with new 3-5 year commissioning plans that will fill a
£30bn “funding gap” by 2020/21. CCGs are supposed to consult with charities and patient groups to find ‘local solutions’ to cutting their share of the £30bn.
Calderdale Council Leader Tim Swift reports on his blog that he calculates this means
Calderdale CCG will lose £80m out of its budget over the period to 2020/21.
Presumably the “local solutions” will fall somewhat short of throwing patients out on the
street. Although, given the record of the Bedroom Tax, I wouldn’t bet on it.
Called to give evidence to the House of Commons Health Committee, the NHS England Chief Sir David Nicholson was forced to admit that NHS England had put aside £3m of taxpayers’ money to produce ‘materials’ for a public ‘consultation’ on how to solve the £30bn funding gap, without telling MPs.
With regard to the £30bn NHS “funding gap” that will open up by 2020/21, Sir David Nicholson told MPs,
“This gap cannot be solved from the public purse but by freeing up NHS services and
staff from old style practices and buildings.”
An article in Pulse said that he then
“remained coy with the committee about exactly what it would entail.”
The NCAT Report says nothing about Calderdale Royal Hospital’s notoriety as one of the most costly, least accountable Private Finance Initiatives in the NHS
Repaying the ever-growing PFI debt currently takes about 10% of Calderdale CCG’s annual budget, and this is set to rise.
At the April 2013 meeting of the Calderdale CCG Governing Body, it was noted that
Private Finance Initiative payments for Calderdale hospital will be £24m this year (they
increase each year) – almost 10% of the CCG’s 2013 annual budget of £256m.
Details of the Calderdale Royal Hospital contract are on a PFI list compiled by the
Treasury. This shows that while the capital cost of rebuilding Calderdale Royal Hospital
was £64.6m, the scheme will end up costing Calderdale and Huddersfield NHS
Foundation Trust a total of £773.2m.
6 community health centres in Kirklees are also PFI schemes, undertaken by Kirklees PCT.
Kirklees PCT was abolished in the 2012 Health and Social Care Act, and as a provider of
NHS community health services it was replaced by Locala, a private social enterprise
company. The total capital costs of the 6 community health centres were £25m but the total unitary charge payments are £89.6m.
The NCAT Report says nothing about how deprivation, austerity and cheap alcohol have
driven the increase in Calderdale A&E admissions.
The final item in this little shop of horrors is the fact that cuts to social care funding and services are a major cause of rising use of A&E.
Restoring social care funding and services seems like a no-brainer. It would not only
cut A&E admissions, it would put wages into the pockets of social care staff that would
in turn fuel the economy. It would also put taxes into the Treasury coffers to pay for
A&E and other NHS and public services, and reduce the public deficit while we’re about it.
Updated 7 March with news of the £1,222,000,000.00 NHS sell off by
NHS Greater East Midlands Commissioning Support Unit. The Supply2Health advertisements for the contracts are here:
https://www.supply2health.nhs.uk/0AK/Lists/Advertisements/DispForm.aspx?ID=60
https://www.supply2health.nhs.uk/0AK/Lists/Advertisements/DispForm.aspx?ID=59
Here is the NCAT Report on Calderdale & Huddersfield A&E, if you want to read it for yourself.
NCAT Report – Calderdale and Huddersfield NHS Foundation Trust A&E by JennyS19
Pingback: ConDems say cut back – we say fight back! | National Health Action Party - Yorkshire
Thanks for this excellent analysis